Terbinafine: An effective drug for many fungi
An infection is defined as the process by which a microorganism invades any part of the human body. These infectious elements can be parasites, bacteria, viruses, and fungi. The Fungi belongs to the group of yeasts, molds, and other fungus-producing organisms.
Healthy human beings have fungi in our bodies; this is called colonization and is necessary to maintain a biological balance. Thanks to this balance of microorganisms our body can defend itself from many harmful influences. For example, Candida provides an optimal ecosystem in the vagina; while Malassezia predominates in the skin. We have more than 60 types of fungi only in the nails, incredible!

Most fungi play an important role in recycling decomposing organic matter and efficiently contributing to balanced biological systems. However, a small number of hundreds of species can behave as dangerous opportunistic fungi causing the annoying diseases.
The story changes when these healthy fungi become a headache, causing infections. Infection takes place when there is a body increase of microorganisms, so much so that it leads to a biological imbalance producing damage as the main consequence of it.
The estimated annual incidence of pathogenic candidiasis is 2-20 cases per 100,000 populations.
We refer to approximate figures because fungal infections are not reportable diseases; their numbers are poorly known, therefore. The highest incidences are found theoretically in countries such as Spain, Denmark, and the United States, according to numerous population studies with similar results.
A fungal infection can be identified by its signs and symptoms, with itching being a distinctive symptom in almost all of them. These symptoms change according to the type of infection.
In ringworm of the scalp, the loss of hair, black spots, flaking, and itching, for example, predominates, while in ringworm of the body, oval and reddish spots with itching and pus secretion appear.
Fungal infections are more common in tropical and subtropical countries than in the rest of the world, although this is not always sustainable; the truth is that heat and humidity favor the growth and spread of fungi.
The treatment of infection always consists of substances that antagonize the invading agent, being the antibiotics in bacterial infections, antiparasitic in parasitic infections, antiviral in viral infections, and antifungal in fungal colonization.
Cleaning the infected area and using powerful drugs are helpful in treatment. Terbinafine is a highly effective antifungal against a variety of pathogens of the Fungi kingdom that attacks nails, hair, and skin. Its effectiveness is attributed to fighting against infections produced by dermatophytes such as Microsporum canis, Trichophyton rubrum, T. tonsurans, T. verrucosum, T. interdigitale, T. violaceum, T. mentagrophytes, and Epidermophyton floccosum, and by yeasts such as Candida albicans and Pityrosporum orbiculare (Malassezia furfur).
What is Lamisil® and how does it work?
Lamisil is an OTC medicine whose main component is Terbinafine, a powerful antifungal that can act in two ways; as a fungicide or as a fungistatic, depending on the germ characteristics and the dosage used.
It is quite interesting the mechanism by which Terbinafine works against fungi, but to understand it well, we must first understand certain points about the properties that define fungi.
In nature, certain living beings have cell walls, while others have cell membranes. Human beings have cells covered by cell membranes, for example, while plants, fungi, bacteria, and algae have cell walls.
The cell wall is stiffer, stronger, and much more resistant, unlike the cell membrane. It is made up of a large number of proteins that give it strength and work as mediators with the outside world.
The primary components of a cell wall are cellulose, polysaccharides, peptidoglycans, chitin, and ergosterol. These chemical elements are what determine the resistance of this cellular compartment.
The cell wall of the fungus has as its principal component chitin and ergosterol. The first is an essential carbohydrate that forms part of the skeleton of many beings, and the second is an analog of cholesterol, primordial for the survival of this organism.
Ergosterol is produced through a complex chemical reaction promoted by the enzyme squalene epoxidase utilizing an important substrate known as squalene.
Terbinafine is an alilamines compound-derived that has a wide pharmacological spectrum, and thanks to its mechanism of action, it can act against several fungi. Now that we know how fungus and their walls are composed, we can talk about the mechanism of action of Terbinafine.
This drug travels throughout the bloodstream to act on the site of infection by attacking the fungus once it is absorbed, but how does it do so? Terbinafine can inhibit the functionality of the enzyme squalene epoxidase, stopping the first step of ergosterol production, which is an essential component in the fungi structure.
Without ergosterol, the fungus cannot survive, as its cell wall is incomplete and cannot provide all the necessary support and transport functions. When a microorganism is missing an essential component for its wall, its metabolic system automatically detects that the cell is abnormal and induces its death.
Terbinafine has two forms of action, the first is known as fungistatic and aims to interfere with the production of the cell wall, and the second is its fungicidal effect.
The fungicidal effect is due to its capacity to induce squalane accumulation inside the fungus. If the main enzyme of this system which uses squalene as a substrate, is inhibited, an excessive quantity of the substrate squalene, takes place.
This excessive accumulation of squalene induces failure of the fungus cellular metabolism resulting in the death of the fungus. Then, depending on the organism found in the infection and the doses used, Terbinafine can be used in two ways to attack the agent; be a fungicide or be fungistatic.
Indications and contraindications:
Its indications change according to the route of administration used.
It is used as a treatment for superficial mycosis of the fingers and nails if taken orally in tablet form, produced by fungi sensitive to the component.
It is mainly indicated as the treatment of ringworm if it is applied topically in the cream form; body, groin, scalp (capitis), foot (athlete's foot or tinea pedis), and tinea versicolor.
Body infections caused by fungi are known as tinea, named for the appearance of skin lesions that resemble moths. The fungi found in these infections that are susceptible to Terbinafine are:
- Tinea corporis affecting extremities and torso: Microsporum, Epidermophyton and Trichophyto.
- Tinea capitis affecting the scalp: Microsporum and Trichophyto.
- Tinea cruris affecting the groin area: Trichophyton rubrum.
- Tinea pedis affecting the feet: Trichophyton rubrum, the Trichophyton mentagrophytes.
- Onychomycosis affecting the nails: Trichophyton mentagrophytes and Trichophyton rubrum.
- Tinea versicolor affecting normal skin pigmentation: Malassezia furfur.
It also has contraindications like other medications that we should be aware of to avoid surprises.
If you suffer from hepatic disorders or your liver does not work well, you should not take Lamisil® or any form of Terbinafine.
Its use is not advised in people with liver diseases causing liver dysfunction, since Terbinafine is metabolized in the liver. Your doctor should make sure that your liver is partially working and that it can metabolize the drug if the prescription is obliged; you must undergo tests of liver function for this.
If during treatment, you experience symptoms such as nausea, vomiting, fatigue, abdominal pain, and sudden unexplained yellowing of the eyes and skin, please discontinue Terbinafine immediately and consult your trusted M.D as soon as possible.
Something similar happens in kidney failure patients. It should be used with caution in people with impaired kidney function, especially those with creatinine clearance below 50 ml/min. Or blood creatinine greater than 300 microsmoles/l. although Terbinafine has not been scientifically proven to affect kidney function.

The possibility of Terbinafine to harm the fetus during pregnancy has not been proved to date, yet it is considered as a risk B drug in pregnancy. Its use is not approved, although there are no conclusive studies about its teratogenicity.
Terbinafine can pass through the small ducts where milk is produced releasing into breast milk; for this, its use is not recommended in breastfeeding women. It should be used only when there are no other options and if is essential.
Side effects:
The side effects of Terbinafine are generally brief and not severe. They can quickly improve until they disappear with small changes in the administration scheme; so, they can be relieved with small doses reductions.
Side effects signs and symptoms can be classified according to its frequency in Usual, Unusual, Rare, and Very rare.
Usual:
The most frequent clinical manifestations involve the tegumentary system, with skin allergies such as itchy rashes and redness to mild hives being the most common. These reactions are usually mild, improving with usual antihistamine medications.
Other common symptoms are those of the gastrointestinal tract: a feeling of fullness, loss of appetite, nausea, abdominal pain, burning and flatulence after meals, and diarrhea.
Other not so frequent clinical signs belong to the musculoskeletal system: You will likely perceive joint or muscle pain in the first weeks of treatment.
Unusual:
In this category fall the clinical symptoms that affect more than 0.1% of patients and compromise mainly the sensory organs.
The sensory organs include the eyes, ears, tongue, and nose, where we see, taste, smell, and hear. During treatment with Terbinafine, you may experience disturbances in taste that can range from a slight loss of taste that recovers in weeks to a sustained loss that recovers in months.
Rare:
They mainly involve the liver and bile ducts. You may suffer damage to the hepatobiliary function represented by acute hepatitis or severe liver failure during treatment with Terbinafine. For this reason, it is NOT advisable to consume Terbinafine in patients with pre-existing liver failure.
Very rare:
Very rare symptoms affect less than 0.01% of patients taking Terbinafine, and those observed so far are severe skin reactions such as Stevens-Johnson syndrome, severe allergic reactions such as angioedema, and certain blood disorders such as neutropenia, thrombocytopenia, and agranulocytosis. The latter are diseases that involve blood cells.
It has been found in other exceptional situations that Terbinafine can cause hair loss; however, it has not been possible to set the precise correlation between the intake of Terbinafine and hair loss. Therefore, it is a fact with a lack of support.
Be sure to consult your doctor immediately if you notice any of the above symptoms. If you experience redness, itching, and swelling of the skin, or changes in your usual digestion, stop taking Terbinafine and call your doctor now.
Interactions with other medications:
Terbinafine is unlikely to interact with other medications when used topically. The real danger appears when mixed with other drugs orally.
Its liver metabolism depends on the CYP2D6 enzyme system, so it interferes with all drugs that follow this same liver step. The medications that use this same system are Dextromethorphan, beta-blockers, tricyclic antidepressants, Venlafaxine, Codeine, Tramadol, and other opioid derivatives, antipsychotics such as Haloperidol and Risperidone, Ondansetron, Chlorphenamine, Metoclopramide, and Tamoxifen.
Some interactions have also been described with caffeine, theophylline, cyclosporine, and galantamine. When Terbinafine is used in combination with galantamine, there is an increase in the blood levels of the latter, evidenced by the appearance of nausea and vomiting.
Experts also explain that Rifampicin can increase almost entirely the Terbinafine blood levels, while Cimetidine reduces them by almost 33%.
Properties of Terbinafine:
Body distribution and metabolism:
This pill travels through the entire bloodstream to the organs of action after its ingestion, where it is concentrated mostly, such as the skin, hair, and nails.
Terbinafine starts working after the first two hours of intake and then increases its levels in the next four hours. Another special feature is that it is largely released in oil, specifically in oily skins, being quite effective in seborrheic skins.
70% of the dose taken is absorbed, and its elimination occurs through the urinary tract 17 hours after consumption.
Dosage plan:
You should be aware that to take this medication you must have previously attended a medical consultation. Do not take Terbinafine if it has not been indicated by your doctor.
Do not take Terbinafine if you suffer or have suffered from liver disease. Do not take Terbinafine if you are allergic to the components of the drug.
Do not take Terbinafine if a friend, neighbor, or family member has recommended this medicine. Only take Terbinafine when your doctor has told you to and has made sure that your liver and kidneys are working properly.
The dosage program depends on the needs of each patient, the goal of treatment, the type of fungus causing the infection, and the expertise of the physician; thus, lower doses are needed in certain people, while higher doses may be required in others.

Lower doses are used in children over 5 years old who weigh between 20 and 40 kg. The approved amount is 125 mg per day, taken once a day.
Higher doses are used in older children, up to 250 mg per day once a day. This item applies to children weighing more than 40 kg.
250 mg is recommended once a day in adults, as well as in older children. Depending on what we mentioned at the beginning, this might not always be the case.
The length of treatment will depend on the severity of the infection and the doctor's prescription. The treatment should last at least 2 weeks and can be extended up to 6 weeks depending on the size of the infection and the damaged tissues near the skin infections; thus, in ringworm pedis, for example, the treatment can last up to 6 weeks.
On the opposite, the recommended treatment duration should be 4 weeks in infections involving the hair and scalp.
Know that when Terbinafine is used topically on the skin, its penetration is low and effective levels are reached at the infection site one week after starting treatment, lasting for 30 weeks after the last application. This is why a prolonged treatment is necessary when used as a cream.
In nail infections the suggested treatment should last between 6 and 12 weeks, very long right? Here we will explain why.
First, we must know what nails are. The se are a thick tegumentary organ, made up of a resistant layer of keratin-filled cells fused into a single smooth mass 1.0 mm thick.
The permeability of the nail is weak compared to the skin due to the thickness and hardness of its structure. This permeability can increase when the nail is hydrated, as well as the skin.
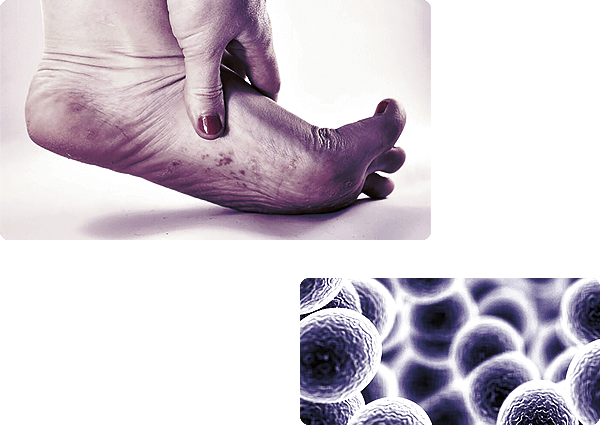
When the nail gets sick -as it happens in fungal infections, onychomycosis- its surface becomes thicker than usual, further reducing its potential to absorb drugs.
Oral treatment (taken) versus topical treatment (applied) is much more effective but more aggressive, in consideration of the long-term duration of the treatment.
No physician would recommend treatments taken for such a long time, and even less so when liver health is at risk.
Topical treatment is preferred because it is less aggressive but equally effective and does not produce as many side effects; the only drawback is that the cream is poorly absorbed.
Long-term, highly effective, harmless topical treatments are chosen, even when they are poorly absorbed all to compensate for this inconvenience.
For this reason, topical treatment should always be the first option in mild or moderate onychomycosis, in children, and people allergic to the components of Terbinafine.
Please, know that people with poor nail growth may need longer treatments, and nail wounds may disappear after several weeks of treatment, even after finishing it.
Efficacy and safety of Terbinafine: Why choose Terbinafine?
The scientific studies that support the clinical use of Terbinafine are numerous; its use in fungal infections is widely recommended since 2015 for its efficacy and safety, as the side effects are mild and potentially reversible.
A comparative study that sought to find out the safety and efficacy of Terbinafine compared to Eberconazole determined that the cure rate of both drugs was similar, reaching 80%. The researchers note that there were no statistically significant differences between the two drugs and that improvements appeared after two continuous weeks of treatment.
Another important research conducted in 2019 sought to compare the efficacy of Terbinafine with Itraconazole. Scientists found that both drugs achieved the same rate of progress in itching, scaling, and redness.
An important fact is that Itraconazole provided moderate side effects such as diarrhea, nausea, vomiting, and abdominal pain during this study, compared to Terbinafine which produced little or no side effects in certain patients. Preliminary results established that both antifungals are equally effective and safe.
A further study carried out in 2019 by Dr. Ting-Hua Yang clarified that Terbinafine is also useful in the treatment of otic mycosis, keeping the function of the ear untouched. This study may be a precursor for others since it was conducted in animals and not in humans.
Additional important data provided by long-term safety and efficacy studies establish that no toxic outcomes have been reported using higher doses of Terbinafine in any of the species, according to animal studies.
A recent study on the carcinogenic potential of Terbinafine showed that it does not produce significant neoplastic effects in mice, which is adaptable to humans. No impacts on fertility or any mutagenic evidence of this drug have been found to date.
Warning signs and treatment of fungal infections
Infections are probably the most usual disease cause in the world and one of the first reasons for medical consultation in the day today. Your doctor for sure has told you that the cause of your general malaise is an infection when you have been ill.
Infection is a process by which a potentially dangerous germ invades our body thanks to its ability to colonize. All germs can multiply and colonize any organism.
These germs have some attributes that make them resistant and capable of adhering to different sites. Bacteria, for example, have essential proteins in their cell wall that allow them to stick to any surface and lengthen their time in the human body.
Our skin and mucous membranes are highly effective barriers against the invasion of pathogenic microbes; otherwise, we would live sick. Humans are in constant touch with bacteria, fungi, and viruses on a daily basis. These germs are on the forks we use even on our toothbrushes, but none are capable of producing disease thanks to our immune barriers.
The infectious disease appears when these natural barriers do not work correctly, either because they are injured, there is a chemical imbalance or because the microorganism has better specific abilities to adhere to the skin and produce disease.
The environment, genetics, and certain situations can contribute to this colonization. Some germs also take profit of their composition to invade and replicate; thus, some bacteria enjoy adhesives that allow them to bond strongly to the skin barriers, while fungi take advantage of their ability to change shape.
Other predisposing factors that influence the onset of infections are age, sex, race, whether there are previous diseases, and the areas where they occur since some infectious happen conveniently when the immune system is depressed or malfunctioning due to other illnesses.
Fungal diseases represent a particularity in the world of infectology since these eukaryotic beings have their own different characteristics that define their behavior and consequent symptoms.
Fungi have existed since the world is a world and have been interacting with humans for millions of years. As a result of this dynamic interaction, some people can respond successfully by destroying the fungus while others develop serious diseases, all depending on immunological capabilities.
These are germs widely distributed in nature; they are in food, vegetation, animals, and meals, and only a few species are really dangerous to humans.
How do fungal infections appear?
The evolution of the infectious process is a bit extensive, but to understand it, we can divide it into a few steps:
The first step depends on the indemnity of the body walls, being the skin, and the mucous membranes the main ones. When these barriers are intact, our organism can successfully respond to daily contact with germs.
The real problem is when these barriers lose their architecture due to damage, whether from injury or trauma. If this happens and there are germs nearby, they stick to the damaged cells thanks to their wall proteins, colonizing the area.
The process of adherence and resistance to physical removal begins once contact with the cells of the host body has taken place. The same proteins mentioned above produces this step. Then the invasion into the host cell begins; competition for nutrients from the healthy cells, and resistance to the body's defense mechanisms.
Fungi make use of healthy cells and their food to survive once they enter the human body, as they cannot by themselves. In this process, the activation of the defense mechanisms of the immune system begins.
The immune system is now activated, and the severity of symptoms depends on how massive and efficient the immune response is. Battle cells are activated that release protective proteins, antibodies, and enzymes in this response.
There is not only protein release, but also cell activation that influences the immune response, thanks to the fact that they induce the activation of other cell groups such as neutrophils and macrophages. That is what produces the typical inflammatory response defined by swelling, redness, increased volume, and itching in some cases.
Of course, not all people get fungal infections; in fact, these types of conditions mainly affect patients with predispositions or risk factors. Patients likely to suffer from a fungal infection include immunosuppressed patients, patients on prolonged antibiotic treatment, patients with immune problems, malnourished patients, patients who have suffered a severe blow or trauma, or elderly patients with a weak immune system proper to aging.
| Drug | Nominal weight (g)* | Mean measured weight (g) | %RSD | Mean percent of target weight | Mean weight loss (%)** | |
|---|---|---|---|---|---|---|
| Proscar® (Finasteride 5mg) | Whole tablet (n=10) | 0.150 | 0.152 | 0.59 | 101.64 | – |
| Half-tablet (n=20) | 0.075 | 0.074 | 37.40 | 99.42 | 0.58 | |
| Quarter tablets (n=40) | 0.037 | 0.035 | 45.79 | 95.51 | 2.22 | |
| Lamisil® (Terbinafine 250mg) | Whole tablet (n=10) | 0.385 | 0.387 | 0.42 | 100.58 | – |
| Half-tablet (n=20) | 0.193 | 0.185 | 7.86 | 98.59 | 3.96 | |
| Quarter tablets (n=40) | 0.096 | 0.092 | 14.78 | 95.90 | 4.09 | |
| * Nominal weight for intact tablets equals the measured weight mean per tablet for the sample and the nominal weight for half and quarter tablets is 1/2 and 1/4 of the determined weight, ** The mean amount of tablet weight loss caused by the splitting process | ||||||
Fungi composition and how they damage cells
From the Latin fungus, a fungus is a eukaryotic organism, meaning that its nucleus is housed in a membranous compartment in the center of its cell. These beings belong to the Fungi kingdom along with yeasts, and mushrooms.
Fungi are widely distributed in nature, and only a few hundred have the pathogenic capacity. Their ability to reproduce is also interesting and has some similarities to humans.
Reproduction can be sexual or asexual. In simple one-celled fungi, reproduction is asexual through a process called budding. In more complex organisms, the process of reproduction is sexual through spores.
Now, how can fungi harm our health? Well, microscopic beings have certain special functions that allow them to injure and produce disease.
Within these functions, we find the ability to produce toxic filaments, the ability to release metabolites, the production of destructive enzymes such as proteases, phospholipases, and elastases, and the release of toxins, the latter is an exclusive capacity of certain microorganisms although.
These germs burst tissues when these substances are free into the keratinized (skin) and non-keratinized (mucous membrane) layers producing wounds and triggering an inflammatory process.
Fungal infection types:
We can group them into three types depending on the area in which they appear being superficial, subcutaneous, and deep.
Superficial mycoses involve the skin, especially the stratum corneum of it and its attachments such as hair and nails.
The fungi that produce skin infections are called dermatophytes. This name comes from their ability to invade keratinized tissues. More than 40 species with pathogenic capacity within this category are known, of which the most relevant belong to three fundamental groups: Trichophyton, Microsporum, and Epidermophyton.
Dermatophytosis, also called dyes or tinea, is a superficial infection that result from damage to the keratin of the skin, hair, and nails. Dermatophyte fungi are named like that for their moth-eaten appearance.
These fungi have a preference for the skin of the body, torso, groin, hairy skin, fingernails, and toenails (athlete's foot), and scalp. Each type of superficial infection is named according to the location where it occurs:
- Tinea capitis or ringworm of the head is the infection that involves the scalp.
- Tinea corporis or ringworm of the body is the infection of the torso and limbs.
- Tinea cruris or ringworm of the groin is the skin condition of the groin.
- Tinea manuum or ringworm of the hand is the infection of the palms and interdigital region.
- Tinea pedis, ringworm of the foot, or the well-known "athlete's foot" mainly affects the feet in the soles and interdigital areas.
- Tinea barbae or ringworm of the chin is the infection of the beard and hairy skin of the neck.
- Tinea facialis or ringworm of the face is the infection of the face.
- Tinea unguium, or ringworm of the nail is the infection of the onychomycosis type nails.
The occurrence of these diseases is cosmopolitan, meaning that there is no predisposition to sex, age, or gender. The truth is that dermatophytosis is more likely to appear in warm and humid climates because these environments favor the dissemination and replication of fungi.
Hygiene also plays a fundamental role in the development of the infection. Mycoses may be more frequent in people with poor hygiene habits.
Subcutaneous mycoses involve the subcutaneous tissue and skin, and the most popular of these is Sporotrichosis. These infections can go beyond the subcutaneous tissue, affecting muscles and the fascias that surround them.
We speak of subcutaneous mycosis because they are intimately related to the dermis, always being its front door, but they extend deep into the muscles and fascias.
We can highlight the sporotrichosis, lobomycosis, rhinosporidiosis, mycetoma, and chromomycosis among them. The distinctive factor of all is that they can produce granulomas and some grades of fibrotic damage.
Deep mycoses represent systemic infections that involve large organs and tissues putting the patient's life at risk. The most frequent pathogens are Candida and Aspergillus.
Profound infections are the result of a depressed, defective, and poorly responsive immune system, which encourages opportunistic colonization by fungi.
There is damage to internal organs such as lungs, heart, bones, muscles, brain, and liver during systemic infection, and the needed treatment must be invasive and intravenous.
How to recognize a fungal infections and when to see a doctor?
There are many forms of expression of a fungal infection; usually itching is a common symptom in almost all of them.
- In ringworm of the head appears inflammation with the formation of reddish plates and fall of whitish scales. There may be hair loss followed by the growth of a large red and well-defined circumference. This type of condition is common in children.
- You can appreciate several forms In the ringworm of the body 1) Lesions in annular shape with raised and reddish edges that detach pus in some cases. 2) A protuberance growth called Granuloma that is located usually in limbs, and 3) Discharge of pustular type lesions with crust formation.
- In the folds ringworm, reddened lesions in areas of folds such as the thighs, groin area, or folds between the fingers are seen.
- In nail ringworm, there is thickening and change in color of the nails, also shows a yellow-white dot on the nail surface. It is more frequent in the foot nails than in the hand nails.
Now for the million-dollar question, is it necessary to consult a doctor? Yes, it is essential to see a specialist whenever there is a clinical manifestation of a fungal infection. Mycoses generally start from the most superficial to the deepest, the fungi first take profit of the natural barriers, and as the infection advances, they get deeper and deeper. The ideal is to act in time.
For this reason, it is necessary to go to a doctor once you have noticed the first symptoms of fungal infection; so you can avoid further complications. Fungus generally does not produce fever or pus; on the other hand, its most common symptom is itching that does not stop easily, even with medication or the fall of unexplained scales.
Your doctor may request laboratory tests, since many infectious diseases are similar to each other, especially those with skin involvement.
The focus of treatment will be on the organism responsible for the infection; fungi and broad-spectrum antifungals are used in this case.
Antifungals can be taken orally or applied topically. Treatment preference will depend on your physician's judgment and the severity and extent of the infection.
Treatment may last from 2 weeks to 12 weeks, depending on the location. In nails, for example, prolonged treatment of 12 weeks or more is preferred by the hardness of absorption of its structure.
A medication that can be applied to the nail surface is always preferred because as the treatment is long, the side effects are less.
Deep fungal infections require either in-venous treatment (when very critical) or oral treatment, depending on the severity. Daily endovenous treatment is necessary for patients needing hospitalization because of vital organ involvement as the brain, heart, and lungs.
We recommend you to collect information about your illness before the medical interview, for example:
- How long ago the symptoms appeared.
- How long you have had the lesions.
- Any medications or foods you took before the appearance of the symptoms.
- Information about your siblings', parents' and grandparents' illnesses.
- Detailed description in chronology and characteristics of your symptoms.
Remember to consult your doctor with any questions or concerns. During the medical interview, you should collaborate by answering correctly the questions the doctor asks you; this will not only help the doctor but also help your diagnosis and treatment.
By: Dr. Cindy Li