Mycoses
Mycoses (fungal diseases) - a large group of skin lesions caused by pathogenic fungi.
Modern classifications of dermatomycoses are based on genus and species belonging of fungi, the depth of their penetration into the affected tissues and the response of these tissues, the fungus' attitude to skin appendages (hair, nails), the predominant localization of mycosis.
Highlight: I. Keratomycoses: multicolored lichen and others. II. Dermatophytosis: inguinal epidermatophytosis; epidermophytosis of the feet; rubrophytosis, trichophytosis; microsports; favus. III. Candidosis. IV. Deep mycosis: blastomycosis, sporotrichosis, chromomycosis and others and pseudomycosis: erythrazma, actinomycosis.
Etiology and pathogenesis
Keratomycoses is understood to be fungal skin diseases in which the pathogens only affect the horny layer of the epidermis and do not cause inflammatory skin reaction.
Dermatophytes are a group of mycoses caused by fungi that affect the skin (usually epidermis) and its appendages (hair and nails). These pathogens include fungi of Trichophyton, Microsporum and Epidermophyton genera.

Unlike other pathogenic microorganisms, dermatophytes grow better at temperatures below human blood temperature. Temperature from 25 to 30°C is optimal for them. They easily tolerate low temperatures and die at high temperatures. A high temperature can therefore be used as an effective disinfection method. A prerequisite for the development and growth of dermatophytes is a humid environment. This is especially true for mycosis pathogens of the feet. This is why infection and exacerbations of the disease are observed in the summer, when the feet sweat increases. Dermatophytes are resistant to UV rays, optimal for their vital activity is a neutral and slightly alkaline environment, shifts in acidity in one direction or another, especially in the sour, have a negative impact on fungi. Some dermatophytes can parasitize only on humans, others - on humans and animals. In this regard, there is a distinction between anthropophilic and zoophilic fungi, respectively. The age of the patient is extremely important for the development of the mycotic process. Trichomycoses (trichophytosis, microsporia, favus) can affect long hair, which causes damage to the scalp and cannon hair when the pathogens spread to smooth skin, and are usually observed in children. Stop mycoses (rubrophytosis and epidermophytosis) are mainly observed in adults. The main role is played by age-related changes in the acid-alkaline balance of the skin, the chemical composition of skin fat. The distinctly acidic reaction of sweat in children under 1-2 years of age, then the acidity decreases, approaching the neutral at the age of 5 to 10-12 years. It is known that in this age period the incidence of trichomycosis reaches its peak. During puberty, the acidity of sweat increases again. In adults on different parts of the skin the reaction of sweat varies widely: on the head, back, chest it is sour, and in the interfinger folds, especially the legs - neutral or slightly alkaline. Of importance is the different chemical composition of sebum secretion in children and adults. Adult hair has fatty acids that have fungiostatic properties, especially in relation to microsporms. Contribute to the development of dermatophytosis reduction of body resistance, malnutrition, vitamin deficiency, debilitating diseases, metabolic disorders, hormonal imbalances, etc. Particular importance is attached to the functional inferiority of the immune system, especially cellular immunity, which explains the high frequency of dermatophytosis in HIV infection and immunosuppressive therapy. Of the external influences contributing to the emergence and development of the mycotic process, the most important are damage to the integrity of the skin, especially in the form of micro-injuries, and factors that increase skin moisture. The maceration of the epidermis and excess moisture, which are most often observed in the folds of the skin and accompanied by the rejection of the stratum corneum, accumulation of gray fluid and alkalization of the environment, create favorable conditions for the penetration of pathogenic fungi into the skin and their reproduction. That's why wearing closed shoes in summer, especially on the rubber sole, socks and stockings made of synthetic fabrics that do not let in sweat, leads to the development of foot mycoses. Special importance in the pathogenesis of dermatophytosis belongs to the specific sensitization of the body, especially the skin, i.e. increased sensitivity to the fungus that caused the disease. This allergic reaction is often preceded by acute and deep forms of dermatophytosis. It manifests clinically in the form of papules, spots, bubbles, small pustules (mikides). Mushrooms are not found in allergic rashes.
Sheaher multicolor
Multicolored lichen (synonymous with branched lichen) - keratomycosis caused by the fungus Rityrosporum orbicularis.
Etiology and pathogenesis. The fungus lives only on human skin in saprophyte or pathogenic form. Contagiousness of multicolored depriving insignificantly small. Long and close contact is necessary for disease transmission. The emergence of colored deprivation as a result of the transformation of the saprophyte form in a pathogenic or infection from the outside contribute to the weakening of the human body's defense mechanisms, primarily the suppression of cellular immunity, as well as increased sweating. The latter may be due to vascular disorders, excessive wrapping, work in hot shops, prolonged use of antipyretics and other reasons. Often, colorful lichen develops against the background of lung tuberculosis, lymphogranulomatosis, and other diseases accompanied by sweating.
Clinical picture. The mouths of salmon-hair follicles serve as a primary localization of the fungus and a source of relapses. Here it multiplies, forming colonies in the form of yellowish-brown dots. By peripheral growth, these initial elements turn into rounded, sharply delineated spots up to 1 cm in diameter. Melding together, the spots form large centers - palm-size and larger. Such centers have festoon shapes, isolated spots are scattered along their periphery. In the long course of mycosis, lesions may occupy vast areas of the skin: the whole back, side surfaces of the body, chest. Usually rashes have yellowish color of different saturation. However, their color may vary widely - from pale cream to dark brown. The surface of the rashes is covered with branched flakes formed as a result of loosening the epidermis horn layer. Flakes are not noticeable with frequent washing, but scraping easily leads to flaking of mucous membranes (Benjieu symptom). Under the influence of insolation and artificial ultraviolet irradiation in the area of rashes intense peeling occurs, which may lead to a cure. The resulting post-eruptive spots retain the color of the unchanged skin, so they appear light against the background of a common tan, creating a picture of pseudolecoderma. The most frequent localizations are on the chest, back, and armpit pits: from here, the rash spreads to the shoulders, side surfaces of the body, and abdomen. Much less often, the rash appears on the hands, legs, neck, face, scalp, genitals; hands and feet are not affected. Subjective sensations are absent. The flow of branched deprivation for a long time, can last for many years. Sick mostly adults; in old age, the disease is usually subject to spontaneous regression.
The diagnosis is based on the clinical picture. To confirm the diagnosis, a Balzer sample is used; lesions and adjacent areas of healthy skin are lubricated with 5% iodine tincture (with a lower concentration of the sample may be questionable) - rash deprivation due to loosened corneal layer is colored more intensely than the surrounding healthy skin. Of additional importance are the phenomenon of Benjet, examination of lesions of the floor with a Voodoo lamp (yellow glow), microscopic examination of scales for the presence of fungi. Differential diagnosis is made with pink pewter, secondary syphilis.
Treatment: rubbing keratolic and fungicidal agents. For limited rashes use 5% salicyl alcohol, sulfuric (3%)-salicyl (5%) ointments 2 times a day for 5-7 days. More effective ointments are mycosolone, triderm, creams clotrimasol, lamisil, nizoral. Rubbing is performed twice a day. In the common variants Demjanovich's method and taking inside systemic antimicrotics nizoral or orungala within 10-14 days are shown. Prevention consists of disinfection of body and bed linen and sweating correction.
Mycoses Stop
Mycoses of feet - a group of dermatomycosis, affecting the skin of the feet. It mainly includes epidermophytosis, rubrophytosis of the feet as the most frequent mycoses of the feet, as well as inguinal epidermophytosis, which may localize the process, and rarer mold mycoses.
This group is distinguished by common pathways of infection, therapeutic tactics, especially for nails affected by mycosis (onychomycosis), and preventive measures.
The spread of foot mycosis is facilitated by the use of public baths, swimming pools, showers without individual special rubber or plastic shoes. Flakes of foot mycosis patients may get on floors, benches, paths, lattices, carpets and bedding, where in conditions of high humidity they can not only survive but also multiply for a long time (especially on unpainted wooden objects). Transmission is possible with the use of wallpaper shoes, footwear. washcloths, as well as objects to take care of nails and foot skin without disinfecting them.
Epidermophytosis foot
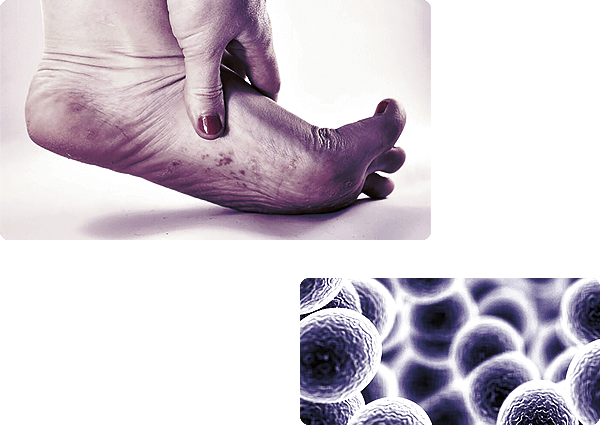
Epidermophytosis of the feet is one of the frequent dermatomycoses that affects the skin and nails of the feet.
Etiology and pathogenesis. The causative agent - Trichophyton mentagrophytes var. interdigitale - is revealed in skin scales, scraps of macerated epidermis, in nail plates in the form of threads of branching mycelium, which often break up into round and square arthrospores; in the material from the nails there are piles and chains of spores. On the environment Saburo colonies have the form of white fluffy lump, gradually becoming powder-like and creamy. The disease is widespread, especially among athletes ("athlete's foot"), as well as soldiers, bath attendants, metallurgists, miners, whose profession is associated with prolonged wear of shoes in conditions of high temperature and humidity, resulting in sweating of the feet. The spread of mycosis is facilitated by poor personal hygiene when using baths, swimming pools, foot sweating, scuffs, micro-injuries, endocrine disorders, immunological failure. The fungus has pronounced allergenic properties, which causes allergic rashes on the skin, facilitates the attachment of pyogenic infection.
Clinical Picture. There are five basic forms of epidermophytosis: erased, squamous hyperatonic, intrigenous, dyshydrotic and epidermophytosis of nails.
The erased form is almost always observed at the beginning of epidermophytosis of the feet. Clinical manifestations are scarce: slight peeling is observed in the interfinger folds (often only in the 4th interfinger interval) or on the soles, sometimes with the presence of small surface cracks.
The squamous hyperatomic shape is manifested by dry flat papules and slightly lichened numeral plaques of cyano-red color, usually located on the vaults of the feet. The surface of rashes, especially in the center, is covered with different thicknesses of scales of grayish-white color; their borders are sharp, on the periphery there is a border of peeling epidermis; single bubbles can be noticed at close examination. Dropping out, serpiginizing and merging, form large diffuse hearths that can spread to the entire sole and side of the feet. When localized in the interfinger folds, the efflorescence may occupy the side and bending surfaces of the fingers, the epidermis covering them becomes whitish. Along with such peeling foci there are hyperkeratotic formations by the type of limited or diffuse omosoles of yellowish color, often with cracks on the surface.
The clinical picture of squamous hyperkeratotic form of epidermophytosis may have great resemblance to psoriasis, eczema and horny syphilides. Dry skin, moderate itching, and sometimes painfulness are subjectively noted.
The intrigenous form is clinically similar to the banal intertrigo. Interfinger folds are affected, the bowl between III and IV, IV and V fingers. It is characterized by a rich redness, swelling, wetness and maceration, often joined by erosion and cracks, quite deep and painful. The intrigenous form of epidermophytosis is distinguished from the banal intertrigo by rounded outlines, sharp borders and whitish fringe on the periphery of the peeling epidermis. These signs allow suspecting the mycotic nature of the disease; the detection of mycelium in the microscopy of pathological material helps to make the final diagnosis. Itching, burning, soreness are subjectively noted.
Dyshydrotic form is manifested by numerous vials with a thick tire. The primary localization is the vaults of feet. The vaults can capture vast areas of soles, as well as the interfinger folds and skin of the fingers; merging, they form large multi-chamber bubbles, at the opening of which there are wet erosion of pink and red color. Usually, the bubbles are located on the unchanging skin; as inflammatory phenomena increase, hyperemia and swelling of the skin join, which gives this type of epidermophytosis similarity to acute dyshydrotic eczema.
Itching is subjectively noted.
Affection of the nails (usually I and V fingers) is found in about 20-30% of patients. Yellowish spots and stripes usually appear in the thicker nails from the free edge; slowly increasing in size, they may eventually spread to the entire nail. The configuration of the nail does not change for a long time, but over the years, due to the slowly growing foot hyperkeratosis nail thickens, deforms and crumbles, becoming as if eaten in the distal part; sometimes separated from the bed. Epidermofitiya moaning. especially dyshydrotic and intrigenous, often (about 60% of cases) is accompanied by allergic rashes, which are called epidermofitides. They can be regional, being located near epidermofitic centers. remote, affecting mainly the hands, and generalized, occupying vast areas of the skin. Epidermofitides are symmetrical and polymorphic: erythematous spots, papules and most often vesicles, especially on the palms and fingers of the brushes.
Rubrophythia
Rubrophythia (rubromycosis) - the most common mycosis of the feet, affecting the skin and nails of the feet, as well as smooth skin and fluffy hair of any areas of the skin, including skin folds, skin and nails of hands.
Etiology and pathogenesis. The causative agent - Trichophyton rubrum - on Saburo environment forms colonies, emitting a bright red pigment, diffusing into the nutrient medium, at microscopy of which fine mycelium and pear-shaped microconidia are detected. Once on the skin, the pathogen may remain in the stratum corneum for a long time, without causing clinical symptoms. The development of the disease is facilitated by increased sweating, poor skin hygiene, endocrine system and metabolic diseases, reduced immunological reactivity. The most frequent routes of infection are the same as in all foot mycoses.
Clinical picture. In the classic form of foot lesions, the skin of the soles is stagnantly hypermised and slightly or moderately lichenified; the corneal layer is diffusely thickened; the skin pattern is reinforced; the surface of the skin is dry and covered, especially in the area of the skin grooves, with floral scales. The lesions can trap the interpallium folds, fingers, side surfaces of the feet and their rear; the nails are naturally involved in the mycotic process. Subjectively, the patient does not experience any anxiety. Rubrophythia of the foot. as well as epidermophythia, begins with an erased form, which then, with the progression of mycosis is transformed into its more active manifestations. An indispensable companion of foot rubroophytosis is the lesion of the nails. And unlike epidermofitniya stop. affecting usually only the nails I and V fingers. with rubromycosis affect all nail plates (and legs, and hands).
There are three types of nail affection: normotrophic, hypertrophic and onycholic.
The normotrophic type changes the color of the nails: in their lateral sections appear spots and stripes, the color of which varies from white to yellow: gradually the entire nail changes color, however, maintaining its shine and unchanged thickness.
For the hypertrophic type, except for the changed color (nails brownish-gray), are characterized by growing undergrowth hyperkeratosis; the nail loses its luster, becomes dull, thickens and deforms up to the formation of onychogriphosis; partially destroyed, especially from the sides; often the patients experience pain while walking.
Onycholytic type is characterized by a dull brownish-gray color of the affected part of the nail, its atrophy and detachment from the bed; the exposed area is covered with loose hyperkeratotic layers; proximal part for a long time remains without significant changes.
Rubrophythia is not limited to the limits of the feet, which is very different from epidermophythia of the feet. Its location outside the feet, the nature of clinical manifestations and their prevalence are subject to very wide variations.
Rubrophythia of hands and feet, smooth skin, skin folds and nails can be distinguished.
Infection occurs as a result of lymphogematogenic spread of fungi from the foci of rubrophythia of the feet, simple transfer by hand or during washing; in rare cases, it occurs primarily when the fungi are introduced from outside.

Rubrophythia of hands and feet mainly affects the palms. The manifestations of mycosis are quite similar to those on the soles, except for poor peeling, which is explained by frequent washing; often there is a one-sided lesion. The nails of the hands are subject to the same changes as those of the feet; primary damage to the nails is possible as a result of intensive and prolonged brushing of the centers of rubrophy of the feet.
Rubrophythia of smooth skin can be localized on any part of the body, including the face; the buttocks, thighs and shins are affected. In typical mycosis variants, it manifests itself in pink or pinkish-red with a cyanidal lump of rounded-up spots, clearly distinguished from healthy skin; the surface of the spots is covered with small scales, along their periphery is an interrupted roller consisting of juicy papules covered (not always!) with small bubbles and crusts. At first, the spots are small (up to the size of coins of different value), increasing in size by peripheral growth and merging with each other, forming vast hearths with festoon contours, sometimes occupying whole areas of skin. Cannon hair may be involved in the process (the mushrooms are located inside the affected hair, which loses its shine, becomes dull and breaks down). Sometimes nodules are formed around the affected hair, complementing the clinical picture of smooth skin rubrophy.
Rubrophythia of large folds (inguinal hips, armpits), often spreads far beyond their limits, is accompanied by itching.
The diagnosis of rubrophythia is based on the clinical picture, data from a microscopic examination of scales, cannon hair, nails. The diagnosis is finally confirmed by a cultural study. Foci of rubrophy of smooth skin differentiate with psoriasis, red flattened lichen, herpetiform dermatitis Duringa, red lupus, etc.
Treatment of mycosis of the feet (epidermophytosis of the feet rubromycosis) usually consists of 2 stages: preparatory and basic. The purpose of the preparatory stage is the removal of scales and corneal layers in the squamous and hyper-hemeratotic form and the elimination of island-inflammatory phenomena in the intrigenous and dyshydrotic, especially in their exematization. Various keratolytic means and methods are used to remove scales and corneal layers depending on their intensity. Arisvich detachment is more effective: an ointment containing 12 g of salicylic acid, 6 g of lactic acid and 82 g of petroleum jelly is applied on the soles for 2 days under the compress. If necessary, the peeling is repeated. A good effect is given by lactic-salicylic collodium (10 g of lactic acid and salicylic acid, 80 g of collodium), which is lubricated the soles in the morning and evening for 6-8 days, then 5% salicylic petroleum jelly is applied to the compress at night, after which leg soap baths and peeling epidermis is removed with pumice. Island-inflammatory phenomena and eczematization in the intrigenous and dyshydrotic variants of foot mycoses are eliminated according to the principles of acute eczema treatment. The main stage of treatment of mycoses moaning is prescription of antimicrotic drugs: lamisil (cream), mycosolone, clotrimasol (cream, solution), mycopolicide, nitrofungin, mycoseptin, Castellani liquid (fukorpin), etc. Treatment of onychomycosis is a difficult task. Lamisil (terbinafine) gives a high level of healing for 6-12 weeks in case of damage to the nails of the fingers of the hands and 12-30 weeks - to the nails of the toes of the feet. The drug is taken inside for 250 mg, local treatment is not carried out.
A more extensive spectrum (including mold fungi, which are often included as a misstinfection) has an orangal, which is administered orally 400 mg per day for 7 days, then after an interval of 3 weeks such a cycle is repeated 1 more (for hand nails) - 2 more (for foot nails) times (pulse therapy). Local treatment is not required.
The first control mycological tests (microscopy and sowing) are performed after 6 weeks of onychomycosis treatment of hands and 12 weeks of onychomycosis of feet. Fungistatic drugs - griseofulvin and ketoconazole (nizoral) - are used in combination with local treatment for onychomycosis of goats. In the 1st month of treatment, griseofulvin is prescribed 6-8 tablets a day, in the 2nd month - the same dose after a day, and then up to the growth of healthy nails 2 times a week. In the treatment with griseofulvin possible headaches, dizziness, pain in the heart area, gastrointestinal disorders (nausea, vomiting, abdominal pain, frequent and liquid stools), toxicodermia. Nizoral (ketoconazole) take 1 tablet (200 mg) per day for 6-8 months or more. Complications and side effects are rare, in 10-14% of cases there is a transient increase in liver enzymes without clinical manifestations of liver function disorders; hepatitis and endocrinopathy are possible. Local treatment of onychomycosis includes removal of nails surgically or by repeated application of keratolytic patches, usually ureaplast (20 g urea, 10 ml water, 5 g wax, 20 g lanolin, 45 g lead patch). The patch is applied for 2 days, then the bed is "cleaned" with a safety razor blade. Later, the naked bed is treated with a variety of antimicrobial agents (salicylic acid and pure iodine 1 g, dimexide 1 ml, distilled water 9 ml; salicylic acid and pure iodine 1 g, dimexide 3 ml, distilled water 7 ml: onychophysian, etc.). After surgical removal, the bed is treated with solkoseryl ointment with 3% ketoconazole (nizorazole) during the 1st week. In outpatient conditions with a small number of affected nails can be recommended daily mechanical aging for a long time with subsequent impregnation with fungicidal liquids (salicylic acid and pure iodine of 1 g, dimexide 30 ml), lacquers, lozeryl, butrafen. Creams of lamysil, mycosolone, triderm, clotrimazole, nizoral and other antimicrobial agents are shown in epidermophytic and rubrophytic folds, as well as limited rubrophytic smooth skin. In case of generalized forms of rubrophy and cannon hair affection, external treatment should be combined with oral application of orungala, lamisil or nizoral.
Prevention of foot mycoses should consist primarily in disinfection of floors in baths, showers, changing rooms in swimming pools and gyms at the end of each working day (preferably boiling water or 1-2% chlorine lime). Water in swimming pools must be chlorinated and regularly changed; ideally, it should be flowing. Wooden grids should be removed from the household and replaced with rubber mats that are easy to disinfect. In enterprises where working conditions require daily showers, all workers should be provided with individual rubber or plastic slippers. Such slippers should also be used when visiting baths and swimming pools. It is very important to strictly monitor the sanitary condition of manicure and pedicure rooms with the obligatory disinfection of instruments after each client, to conduct regular inspections of the workers of baths, swimming pools and showers to avoid mycosis of the feet. Do not use general shoes, socks, and stockings.
Inguinal epidermophytosis
Inguinal epidermophilia - dermatomycosis, affecting the epidermis, less often nails.
Etiology and pathogenesis. Pathogenesis - Epidermophyton floccosum fungus, in skin scales and nail particles the fungus is revealed in the form of septized branched short (2-4 microns) mycelium and chains of rectangular arthrospores. On the Saburo environment, the colonies have a rounded shape, yellowish color and fluffy consistency. Infection occurs through household items used by the patient (sponges, glues, thermometers, underwear), as well as when the rules of hygiene in baths, showers, swimming pools. The development of the disease is facilitated by increased sweating, high temperature and humidity of the environment, damage and maceration of the skin. Men are sicker more often.
Clinical picture is characterized by the appearance of peeling pink spots on the skin up to 1 cm in diameter, gradually growing along the periphery with a simultaneous reduction (up to resolution) of inflammation in the center, resulting in the formation of large (up to 10 cm in diameter) ring-shaped inflammatory spots of red color, forming at the confluence of festoon centers. The borders of the centers are sharp, underlined by edgy bright hyperemic inflammatory roller with bubbles and small pustules on its surface. The most frequently affected are inguinal areas (which is reflected in the name of the mycosis), scrotum, inner thighs, less often the interannual fold, armpit areas, folds under the mammary glands. The interfinger spaces of the feet are much less often affected and very rarely - the nails. Itching is a worry.
The diagnosis is based on the clinical picture and the discovery of the causative agent in a microscopic examination of skin and nail scales. The diagnosis is finally confirmed by a cultural study. Differential diagnosis is made with erythema, rubromycosis, psoriasis, candidiasis.
Treatment: in the acute period, admixtures from 0.25% silver nitrate solution, 1% resorcin solution, ointments mycosolone, trederm, intravenous antihistamines are used, after the elimination of vesiculation 2% iodine tincture, 3-5% sulfur-degty ointment is used, as well as official antimicrobial external agents - mycoseptin, lamisil, clotrimazole, nizoral, etc. are used.
Prevention is to observe the rules of personal hygiene, to fight sweating. Public prevention, as in mycoses of the feet.
Microsports
Microsports - contagious dermatophytosis, affecting smooth skin, scalp, long and fluffy hair.
Etiology and pathogenesis. The disease is caused by Microsporum fungi that have small spores. The etiological role of Microsporum fungi in human and animal pathology is different. In Russia, microsporum is caused by the zoophilic M. canis and the more contagious, though less common, anthropophilic M. ferrugineum. The main sources of M. canis are cats (especially kittens) and dogs, the transmission of the pathogen from which usually occurs by direct contact; infection is possible through objects and things contaminated with scales and hair containing mushrooms. The source of M. ferrugineum is only a sick person, often a child. The routes of transmission of zoophilic and anthropophilic microsporums from a sick person to a healthy person in the family, hairdressing salons, and children's groups are the same as the pathogens of surface trichophytosis. Microsporia is a childhood disease found in children from 4 to 11 years of age, but young women with thin and delicate skin may be affected. In the development of the disease are important hypovitaminosis, immunodeficiency conditions, failure to observe the rules of personal hygiene. The incubation period is 3-7 days.
Clinical picture. In microsporia of the scalp part rounded, sharply delimited large (diameter up to 2-3 cm and more) hearths are formed, the surface of which is covered with a layering of rather densely seated branched scales of grayish-white color on the background of poorly expressed erythema. Its most characteristic feature is a continuous breakage of the hair in the hearth at a height of about 3-5 mm above the skin: the affected hair - it is clearly visible even to the naked eye - is surrounded, like a clutch, grayish-white garment, which is revealed in a microscopic examination of small (such as mana grits) spores of mushrooms surrounding the hair (ectotrix). In the microspore of the hair part of the head, caused by M. ferrugineum, there are multiple foci of small size, irregular outlines, with unclear boundaries. The predominant localization of lesion foci is the edge zone of the scalp with an infrequent spread to smooth skin. Hair breakage occurs at a level of 6-8 mm. Clinically, smooth skin microsports is characterized by mildly inflammatory pink peeling spots with a diameter of 0.5-2 cm with clear boundaries, as they grow, the central part of the spots becomes lighter, and in the peripheral zone can be seen a few papulescent and papulesicular elements. In the future, a new ring (double, triple) may form in the center of such ring-shaped elements, rashes grow and quickly disperse on the skin (especially after washing). Foci of lesions are more often localized on the torso, face and upper extremities. The mycotic process extends to cannon hair.
Diagnosis of microsporia is usually easy and based on clinical, microscopic (detection of fungi in hair and scales) data, as well as the green glow of the lesions in the rays of the Voodoo fluorescent lamp. Differential diagnosis is made with trichophytosis, psoriasis, alopecia.
Microsporia is treated with griseofulvin in a dose of 20-22 mg/kg of child body weight.
The affected hair is removed with tweezers under the control of a Vooda fluorescent lamp. Hair around the hearths is shaved. Locally apply 2-5% iodine tincture, salicylic (2%)-sulfur (5%)-degtyar (5-10%) ointment, periodically perform detachment of Ariyevich ointment (in half concentration). Clotrimasol, lamisil and other antifungal ointments are also prescribed for smooth skin areas.
The treatment continues up to 3 times negative tests for fungi, conducted once in 7 days, and after the first negative test grizeofulvin is taken 2 weeks later, after the third - 1 time in 3 days another 2 weeks. In some cases, they use lamisil, orungal, nizoral inward.
Prevention consists of examination of children in children's institutions in order to identify cases of microsporia, treatment of patients and examination of contact persons with the use of a Vood lamp, disinfection in microsporia foci with quarantine, veterinary care for stray animals (cats, dogs), and sanitation work with the public.
Trichophytosis
Trichophytosis is an infectious dermatophytosis that affects smooth skin, scalp hair, long and fluffy hair, nails.
Trichophytosis is a distinction between superficial and infiltrative, which are independent diseases caused by different pathogens with different epidemiology and clinical picture.
Trichophytosis superficial (anthroponosis)
Etiology and pathogenesis. Pathogens are anthropophilic fungi Trichophyton violaceum and Trichophyton tonsurans. The source of infection are young and middle-aged children suffering from superficial trichophytosis; adolescents and adults (usually women), most of whom have chronic trichophytosis. Infection occurs through direct contact with the patient or through headgear, bedding, combs, combs, hair clippers, and other items and things used by the patient. Usually mycosis is transmitted in a family with a patient with chronic trichophytosis; it may be transmitted in hairdressing salons, kindergartens, boarding schools, schools, and other children's institutions. Long-term contact with the patient, weakened immune protection, and damage to the corneal layer of the skin contribute to the infection. The causative agent may spread not only through the skin, but also lymphatically, for example, in chronic trichophytosis, which usually occurs in women with endocrinopathy.
Clinical picture. Depending on the localization, superficial trichophytosis of the scalp and smooth skin is distinguished.
Surface trichophytosis of the scalp is first characterized by single and then multiple foci with diameters from 1 to 2 cm. One of the foci is 3-4 times larger, with irregular outlines and fuzzy borders. Foci are isolated, with no tendency to merge with each other; the skin in the region of foci is slightly puffy and hyperemic, covered with branched scales of grayish-white color, layers of which may give the focus a whitish appearance; hyperemia and puffiness increase, joined by bubbles, pustules, crusts, especially but the periphery. Within the focus, hair breaks down at 2-3 mm from the skin surface or at the root itself. Diagnosis always requires laboratory confirmation. Differential diagnosis with microsporiasis is only possible with a microscopic examination of the affected hair (the fungus spores are located inside the hair by chains - endotrix) and examination of the child's head under a fluorescent lamp (no glow characteristic of microsporiasis).

Surface trichophytosis of smooth skin can be isolated or combined with the lesion of the scalp. Localized mainly in open areas of the skin: face, neck, forearms, and torso. The disease begins with the appearance of one or more oedemas and therefore slightly protruding over the level of the surrounding skin spots of pink and red color, correct rounded outlines, with sharp borders. Their surface is covered with scales and small bubbles, quickly dried into crusts. The center of defeat becomes a ring with time. Trichophytosis is chronic in adults, mainly in women (80%), has poor clinical manifestations. Included in the process are isolated or in various combinations of scalp, smooth skin (more often than buttocks, thighs) and nails (usually fingers). When making a diagnosis of chronic trichophytosis take into account the long course, the absence of signs of acute inflammation, peeling with scarce dry scales and, most importantly, the presence of "black spots" on the scalp and atrophy sites up to 0.5 cm in diameter. The diagnosis is confirmed by the results of laboratory tests.
Trichophytosis infiltration-forecasting
The infiltration-forecasting trichophytosis is more often observed in rural areas.
Etiology and pathogenesis. The disease is mainly caused by Trichophyton mentagrophytes var. gypseum and Trichophyton verrucosum, which belong to zoophilic fungi.
They usually parasitize on rodents (mice, including laboratory, rats, etc.), cows, calves, less often on horses, sheep and other animals. Infiltrative-negative trichophytosis often acts as an occupational disease, especially in cattle breeders. The source of infection are sick animals, less often a sick person.
The clinical picture of infiltrative and predictive trichophytosis is characterized by sharply pronounced inflammatory phenomena reaching the stage of purulence, and short (up to 2-3 months) cyclic flow, ending in complete recovery without a tendency to relapse. The process may involve smooth skin (usually open areas), scalp, beard and mustache area (parasitic sycose). With the development of suppuration, the foci acquire the appearance most typical for infiltrative-forecasting trichophytosis. On the scalp, beard and mustache area, they are sharply delineated hemispherical or flattened nodes of blue-red color, lumpy surface of which is covered with osteopolliculites, erosions, and sometimes ulceration, crusts and scales. Part of the hair falls out, part of it is loosened and easily removed. A characteristic feature is the sharply dilated mouths of hair follicles, made of pus that stands out when pressed in the form of abundant droplets and even pods. At first, the dense consistency of the nodes becomes soft and doughy with time. These hearths on the scalp resemble honeycomb (kerion Celsi, and in the beard and mustache area - wine berries. The smooth skin is dominated by flat plaques, sometimes very large, with isolated peripillary papules on the surface, transformed gradually into pustule elements. The developed suppuration causes the death of mushrooms. They are preserved only in the scales at the periphery of the lesion centers, where they are found during microscopic examination, the fungus spores are located in chains of the ectotrix type. The outcome of the disease is scar formation. As a result of strong immunity arising in infiltrative-negative trichophytosis, there are no relapses.
The diagnosis is based on the clinical picture, the results of microscopic and cultural studies. Differential diagnosis is made with microsporia, pyodermia, psoriasis and others.
Treatment: prescription of grizeofulvin and nizoral inward. Daily dose of grizeofulvin in all forms of trichophytosis is determined at the rate of 16 mg of the preparation per 1 kg of body weight.
In this dose, the drug is taken daily until the first negative microscopic examination for fungi, which usually takes 3-4 weeks, then 2 weeks after a day and then another 2 weeks once in 3 days. Treatment is considered complete with three negative results of the study conducted at intervals of 5-7 days. Nisoral is administered to adults and adolescents 200 mg (1 tablet) per day, to young children - 100 mg. The duration of treatment is up to 2-3 months. Criteria of healing are the same as in the treatment with griseofulvin. It is possible to use lamisil and orungal. Hair in the lesions on the head is shaved once a week. Local treatment consists in lubricating smooth skin and scalp with 2-5% iodine alcohol solution in the morning and micozolone in the evening. Sulphuric (10%)-salicyl (3%), sulfur (5%)-degtyar (10%) ointments and Wilkinson ointment are used. With sporadic foci on smooth skin, treatment is limited to external remedies with obligatory removal of cannon hair with epilation tweezers.
Prevention of zoonotic trichophytosis consists in the identification and treatment of sick animals and deratisation; these measures are implemented in conjunction with the veterinary service. Anthroponosis trichophytosis involves examination of family members and children's groups, treatment of identified patients, and disinfection in the focal area of trichomycosis. Hairdressing salons after each client require disinfection of instruments and regular sanitary cleaning of the premises.
Favus
Favus is a rare malocontagious dermatophytosis that affects the scalp, long and fluffy hair, smooth skin, nails and internal organs. It is found sporadically on the territory of Russia.
Etiology and pathogenesis. Pathogenesis is anthropophilic fungus Trichophyton schonleinii. The conditions of long and close contact are necessary for disease transmission, which explains the family nature of this infection. Favus usually occurs in children; however, it often affects adults, who are the main source of infection.
Clinical picture. The lesion is usually limited to the scalp, relatively rarely to the nails and even less rarely to smooth skin and internal organs.
The faunus of the scalp runs in typical (scutular) and atypical (squamous and impetiginal) forms. Pathognomonic sign is also typical and forms - the so-called scutulas (shields) arising from the introduction of the fungus into the hair follicles and its subsequent reproduction in the corneal layer. The cheekbone consists of a pure culture of the fungus and is a rounded formation of ochre-yellow color, dense consistency, dry to the touch. The central part of the cheekbone with the hair that stands out of it drops, and the rounded edges are slightly elevated, which makes the cheekbone similar to a saucer.
The lower surface of the cheekbone is convex, the diameter varies from 2-3 mm to 1.5-2 cm, which depends on the age of their existence. After removing the cheekbone, a pinkish-red moist depression is found underneath it. Scar atrophy remains in place of the resolved cheekbones. The hair loses its shine, becomes dusty, ashy-gray, reminiscent of old wigs. They are easy to pull out, but unlike trichophytosis and microsporia do not break. With a common favaux, a kind of "mouse", "barn" smell comes from the affected head. Subjective disorders usually manifest themselves in a slight itch. In the squamous form, abundant scales of whitish-yellow color predominate, sitting quite tightly on the hyperemic skin. In the impetrigenous form, pustules appear in the mouths of hair follicles, quickly drying up into a massive solid yellow peel. The faunus of smooth skin usually develops as a result of the transfer of infection from the affected scalp, but may be isolated. The process begins with the appearance of spots very similar to those of surface trichophytosis. Later on, they form typical macular stumps that tend to grow peripherally and merge with each other. Usually, the faveus of smooth skin has a local character, affecting most often the face, neck, arms and legs, and in men and the reproductive organs. The diagnosis of faveus in typical cases is simple, in atypical cases it causes difficulties, sometimes large. In the absence of cheekbones, the diagnostic role is played by peculiarly changed hair. In all cases, laboratory confirmation of the diagnosis is necessary - microscopic examination of the hair and scales to identify the pathogen that is located inside the hair.
Treatment: similar to trichophytosis.
Prophylaxis. Detection and treatment of patients with faunus with examination of persons who are in close contact with the patient. Disinfection of the focus of infection.
Candidosis
Candidosis (synonymous with candidiasis, moniliasis) - a disease of the skin, mucous membranes and internal organs, due to the pathogenic effects of yeastlike fungi of the genus Candida.
Etiology and pathogenesis. Cansisa fungi belong to conditionally pathogenic microorganisms. They are widely distributed in the external environment; they vegetate mainly in the soil of meadows, orchards and vegetable gardens, on the bark of fruit trees, as well as on fruits, vegetables and fruits, especially stale; they can easily be found on household items, primarily used in the care of infants. As saprophytes, they live on the skin and mucous membranes of a healthy person; they are isolated from excreta, urine, sputum, various excreta and nails with different frequency.
Yeastlike fungi of the genus Candida are single-celled plant microorganisms of rounded, oval or elongated shape with a diameter from 2 to 5 microns, do not have true mycelium, but form pseudomycelium, whose threads are deprived of a common shell and partitions, and consist of thin cells.
C. albicans cells have a six-layer wall, a cytoplasm with glycogen rosettes and a large number of ribosomes, central and several small vacuoles limited by the membrane, mitochondria, a large nucleus limited by the nuclear membrane. Yeastlike fungi have the ability to repel blastopores. Prolonged perseverance inside epithelial cells and even multiplying in them, surrounded by a dense microcapsula fungi are to some extent protected from the effects of drugs, which may be the cause of ineffective treatment. The depth of introduction of elements of yeastlike fungi into the affected tissues varies. For example, in the epithelium of the vagina they penetrate its entire thickness, including the basal layer, and in the oral cavity they are localized in the surface epithelial cells. Candida mushrooms are aerobes. Sugar is especially readily absorbed for nutrition, which can explain their tropism to tissues rich in glycogen, and frequent candidiasis in diabetes. Optimum temperature for the growth of fungi 21-27 ° C; they grow well at 37 ° C; favorable for their reproduction pH 5,8-6,5 and high humidity: drying is tolerated well, can withstand competition with many microorganisms in food, when boiling die within a few minutes. Candidosis can develop either through external infection, or through its own saprophytes. The latter route clearly prevails. Under certain conditions (exogenous - mechanical and chemical injuries, high humidity, etc.; endogenous - immune failure, childhood and old age, metabolic disorders, diabetes mellitus and other endocrine diseases, hypovitaminosis, general severe infections, pregnancy, prolonged use of corticosteroids, antibiotics, etc.) mushrooms can acquire pathogenic properties. In this case, fungus blastospores begin to multiply intensively, forming, along with kidney cells, numerous filamentous forms (pseudomycelium). Fungus pathogenic cells attach to the cells of the epithelium of the mucous membrane, infiltrate them, parasitize in their cytoplasm and nuclei, destroying the host cell, stimulate the production of various antibodies in the human body. Thus, candidiasis is an autoinfection in the vast majority of patients. This fact can be explained by its multi-focus and chronic recurrence.
Clinical picture. The following forms of candidiasis are distinguished: oral candidiasis, urogenital candidiasis, oral corner candidiasis, heilitis candidiasis, smooth skin, onychia and paronichia candidiasis, chronic generalized candidiasis.
Oral candidiasis (candidiasis stomatitis, thrush) is common in infants. The disease occurs in the first weeks of life, usually in premature, carried and weakened children, as well as those born in pathological births. Infection of newborns occurs from a sick mother in the antenatal (prenatal), residential (when the fetus passes through the birth path) and postnatal (up to 7 days after birth) periods. In subsequent periods of childhood the source of infection may be persons from the child's environment, household items and food. Oral candidiasis begins with hyperemia and swelling of the gums, mucous membranes of the cheeks, tongue, less often hard and soft sky, temples and tonsils, capturing over time vast areas; total defeat is possible. Then, against this background appear 1-3 mm in size isolated cottage cheese deposits of whitish color, consisting of vegetation of mushrooms. Over time, their number increases, they increase in size and, merging, form films of varying sizes and shapes of shiny white, grayish or yellowish color. The films are relatively easy to remove without damaging the subject mucous membrane, which retains a smooth surface and red color. Candida stomatitis occurs without general disorders, temperature reactions, regional lymphadenitis and subjective sensations. The course of the disease in children is more often acute and less often chronic. In the chronic course, the lesion may spread to the mucous membranes of the nose (candida rhinitis), vocal chords (voice becomes hoarse, aphonia is possible), lips, throat, esophagus and even the stomach.
In adults, candidiasis of the mucous membrane of the mouth is much rarer, it often occurs under the influence of trauma to the dental prosthesis. It usually takes a chronic course, in which hyperemia and swelling of the mucous membranes decreases, and plaque becomes thick and rough, sometimes resembling leukoplakia. The raids adhere tightly to the mucous membrane and when removed, which is possible with a certain amount of effort, they leave erosion. The tongue is often covered with numerous deep grooves, running longitudinally and transversely, at the bottom of which at the expansion of their edges is found white patches. The tongue may grow in size and, in the words of patients, "fills the entire mouth. Dry mouth, burning, increased with spicy and hot meals are subjectively noted.
Urogenital candidiasis is manifested in the cup in the form of candidiasis balanitis or vulvovaginitis (acute or chronic). Candidotic balanitis is often combined with candidiasis urethritis and occurs as a result of the infestation of the pathogen, often from the rectum, the mouth. The mucous membrane of the penis head becomes red, shiny with erosions, small pustules and curdy whitish plaque. Vulvovaginitis candidiasis is characterized by curdy discharge from the genital tract, itching, burning. The vagina, its anteroom and vulva are hyperemic with the presence of whitish spots and small pustule satellites on the periphery of the hyperemic centers.
Candidosis of the corners of the mouth (candidiasis) occurs as a result of the spread of the disease from the mucous membrane of the mouth, but may be isolated; the lack of vitamins, especially riboflavin, plays a significant role in the development of the disease. As a rule, both corners of the mouth are affected. The mucous membrane in the transition area of the fold is slightly infiltrated, has a grayish-white color, in the depth of the fold is almost always located pinkish-red erosion or crack. Boundaries are clear. The lesion may extend to skin areas adjacent to the corners of the mouth, resulting in infiltration, pinkish-red dyeing and peeling. The periphery of the focus is marked by the fringe of the peeling cornea layer. Meals are usually observed in children, mostly between the ages of 2 and 6. It is rare in adults, mainly in elderly, weakened women.
Heylite Candida (Lip Candida) is characterized by puffiness and cyanosis of the red lip border and its poor peeling, thin lamellar scales of grayish color with freely raised edges. The skin of the lips is thinned and assembled into delicate radiar folds. A slight burning, sometimes painful, is subjectively noted. Candidotic heilitis has a chronic recurrent course, is usually found in older children and adults; it is often combined with jams.
Candidosis of skin folds is characterized by the appearance of small bubbles with a thin flabby tire at the depth of the folds; soon they open with or without preliminary pustularization. The resulting erosions rapidly increase in size and, merging, form extensive erosive areas that may fully occupy the contact surfaces of the folds. The clinical picture of fold candidiasis at this stage is very typical: the erosive areas have a crimson color with a cyan or livid tint; their wet surface has a characteristic lacquer shine. The erosions are clearly delineated from the surrounding healthy skin, passing along their periphery with the narrow fringe of the white peeling epidermis. In large skin folds (intercostal, inguinal and hip, etc.), erosive areas often alternate with areas of macerated epidermis, which is characterized by white color and a noticeable thickening. Erosion and maceration of the epidermis is usually limited by the contact surfaces of folds. On the adjacent to the main lesions of healthy skin can almost always be found in a certain amount of sifting in the form of small bubbles, pustules or erythematosan scamosis rashes. The interfinger folds of the brushes are often affected. This type of candidiasis is found, with rare exceptions. in adults, and as a rule, women, many engaged in domestic work or working in food processing plants for fruit and vegetables, as well as in confectionery factories. Usually one interfinger fold is affected, more often on the right hand. In women, candidiasis of the inter-finger and inguinal thigh folds is usually combined with genital lesions and is accompanied by excruciating itching.
Paronychia and onychia candida (nail rolls and nail candidiasis) occur as a result of local trauma, humidity and maceration. At first, the nail roll is affected. At the place of introduction of the fungus, usually at the edge of the roll, on the border with the nail, there is hyperemia and swelling, which become more and more intense and cover the entire roll. Clinically, at this initial stage, it appears pinkish-red and thickened, to the touch pasty and painful. Over time, the acute phenomena subsides and the paronichia takes a chronic course, the epiphanychium (the nail cuticle) disappears, and there are no purulent discharges under pressure on the inflamed roller of the nail (unlike the streptococcal paronchia). The nail becomes dull and thickened, covered with transverse brownish grooves.
Candidosis of smooth skin develops, as a rule, secondary, with the spread of the process from the skin folds of mucous membranes or pericarpendinous rolls, is characterized by a large variety of clinical manifestations. In typical cases, the disease usually begins with the appearance of abundant small bubbles with a sluggish tire, which are more resistant than similar bubbles in the localization of the process in the folds. In recent years, numerous atypical variants of candidiasis of smooth skin have been described. Its manifestations are quite unusual: folliculitis, papillary papules, etc..
Candidosis chronic generalized (granulomatous) develops in childhood. Of particular importance is the lack of immune protection (especially T-cell protection, which in turn is due to the absence or sharp decrease of anticandidotic IgA in saliva, as well as a violation of the function of neutrophils of m macrophages, The endocrine disorders (hypoparathyroidism, hypothyroidism, diabetes mellitus) of the genus Candida, which leads to the generalized character of the lesion with the development of a peculiar reaction to the candidiasis infection of granuloma type. The process usually begins with candidiasis of the oral mucous membrane, followed by lips, scalp, genitals, hip skin, pubic area, nail rollers, nails, etc. The process involves the following. Typical for the formation of infiltrated erythematous comatose hearths, reminiscent of psoriasis or pyodermia. Visceral candidiasis may develop in the form of candida pneumonia, kidney, liver, eye, heart and fatal candida sepsis.
The diagnosis of candidiasis is made on the basis of clinical data, microscopy of characteristic pseudomycelia and a large number of kidney cells (blastospor) in native preparations or smears (Romanovsky-Gimza, Gram, Tsilu-Nilsen), prepared with whitish plaques from the mucous membrane and skin. The cultural study is used to clarify the species composition of mushrooms. Identification of C. albicans strains is also done with PCR. Isolation of more than 10 CFU from 1 ml of the first portion of urine testifies to the presence of candidacy.
Serological reactions are also used to diagnose candidiasis: agglutination reaction (RAG), complement binding reaction (PCR), precipitation reaction (RP), passive hemagglutination reaction (PHA). IgE against C. albicans is determined in vaginal flushes in women by immunoassay (ELISA).
Treatment: elimination of factors contributing to the development of candidiasis; diet with the exception of sweets, restriction of carbohydrates, rich in proteins; vitamins B2, B6, C and PP. In light versions of candidiasis, skin and mucous membranes are restricted by external medications: cream, pymafucin suspension, creams and ointments - mycosolone, myconazole, econazole, lamisil; clotrimazole solution; 5-20% solution of sodium tetraborate (borax) in glycerine, 1-2% aqueous and alcohol solutions of aniline dyes (diamond green, methylene blue, gentian violet), mycoseptin, nystatin ointment, etc.). The drugs should be applied to lesions 2 times a day (creams and ointments slightly rubbed) until the complete regression of clinical manifestations, then, reducing applications to 1 in 2-3 days, continue treatment for another 2-3 weeks. Treatment of acute forms of urogenital candidiasis is also usually limited to local medications.
Treatment of chronic recurrent urogenital candidiasis should be comprehensive: along with local treatment, immuno, vitamin therapy (group B) prescribe one of the systemic antimicrotics: ketoconazole (nizoral, oronazole 0.2 g), 1 tablet 2 times a day for 5 days; itraconazole (orungal) 200 mg per day for 3 days; fluconazole (diflukan - capsules of 0.05 g, 0.15 g, 0.1 g, 0.2 g, solution for intravenous administration is used once in a dose of 150 mg); natamycin (pymafucin 0.1 g) 1 tablet 4 times a day for 7-12 days; sometimes local treatment (1% butrafen cream) is combined with taking inside one capsule (150 mg) of fluconazole. Systemic treatment is shown for common candidiasis, severe and persistent candidiasis, and failure of external therapy. Three groups of antifungal agents are used: triazoles, imidazoles and polyene antibiotics. Of triazoles, fluconazole (diflukan) is used in a dose of 50-100 mg per day (in the form of gelatin capsules, syrup or solution for intravenous administration containing 2 mg/ml of fluconazole) or truconazole 100 mg per day for 7-14 days. In common (systemic) candidiasis, the daily dose is 400 mg of fluconazole on the 1st day and 200 mg on subsequent days. Nisorazole is widely used - 200 mg/day, at persistent forms the daily dose is increased to 400 mg. Treatment is continued until recovery. Polyene antibiotics nystatin and levorine are prescribed 10 000 000-12 000 000 and 5 000 000-6 000 000 units per day in 3-4 doses during 2-4 weeks, repeated courses are conducted at intervals of 8-10 days. Good results are obtained with terbinafine (lamisil) both in general (250 mg once a day) and in local (1% cream) use. Orangel is the most active.
Prevention of candidiasis is to prevent its development in people at risk - patients with immunodeficiency conditions, blood diseases, neoplasms and other serious pathologies, as well as those who received ionizing radiation, who have undergone massive treatment with antibiotics, corticosteroid hormones and other immunosuppressants. If they are found to have mykonositelstatin for 3-4 weeks, 2 000 000 units of nystatin or 100 mg nizoral per day. Special attention is paid to correction of intestinal dysbacteriosis, treatment of sexual partners in case of genital candidiasis, detection and treatment of candidiasis in pregnant women and infants, and elimination of relevant hazards at work.
Deep mycoses
The group of deep mycoses includes diseases, which are mainly spread in South America, Africa, the USA, in Europe, including Russia, there are only sporadic few cases of this group, except actinomycosis, which is currently classified as pseudomycosis.
The group of deep mycosis includes North American blastomycosis, keloid blastomycosis, sporotrichosis, chromomycosis, and a number of others. Typical feature of deep mycosis can be considered their weak infectivity, the spread of these pathogens in the soil, plants as saprophytes, mainly in tropical climates.
Infection occurs when skin injuries, scratches, cracks are infected. The clinical picture of deep mycoses is dominated by morphological elements such as tubercles, nodes prone to disintegration with the formation of ulcers and lesions of deep layers of skin, subcutaneous tissue, subject muscles, bones, internal organs, which determines the diversity of the clinical picture and sometimes severe general symptoms that do not exclude lethal outcomes.
North American Blastomycosis (synonymous with Blastomyces dermatitidis) - deep mycosis caused by Blastomyces dermatidis is characterized by torpidally flowing ulcerative granulomatous lesions of the skin, mucous membranes, less frequently bones and internal organs. The clinical picture is initially characterized by nodular-pustule elements, which are quickly merged and removed with the formation of vegetative ulcers of bright red color, often with a warty component, cup ulcers are localized on the extremities. From the bottom of the ulcer released viscous blood-purulent exudate, which dries into the crusts. In place of ulcers remain deep scars.
The diagnosis is confirmed bacterioscopically and culturally.
Treatment: amphotericin B, iodine preparations, orungal, fluconazole.
Keloid blastomycosis (Lobo disease) - deep mycosis caused by Clenosporella loboi, is characterized by a relatively benign course with deep skin lesions more often in the foot, shin, less often in the face. Initially, small cyano-red bumpy elements appear at the site of infection introduction, gradually turning into drain nodes with a tendency to necrosis and ulceration. Sores are covered with purulent plaque and warped sprawl. Painful coarse chiloid scars are formed in their place. Diagnosis is confirmed bacteriologically and culturally.
Treatment - amphotericin V. nizoral, orungal, fluconazole, surgical dissection of foci.
Sporotrichum schenckii is a deep mycosis that affects the skin, subcutaneous tissue, mucous membranes, lymphatic system, less often bones and internal organs. It is found as a professional disease in workers' plant nurseries. The entrance gate is micro-injuries to the skin and mucous membranes, infection is possible through the respiratory tract and digestive tract. A distinction is made between sporotrichosis localized subcutaneous, disseminated gum disease, visceral (systemic). Dense red-brown tubercles appear at the site of the fungus introduction, which increase in size by mating with surrounding tissues, and, removing themselves, form "sporotrichoses shankras" - ulcers with uneven papillomatous sprawl and subverted edges. Then, in the course of lymphatic vessels appear tubercles and gummosis nodes, also prone to decay. Hematogenic metastasis of the causative agent with the formation of cold abscesses with fistulous movements and long-lasting nonhealing ulcers is typical for the disseminated sporotrichosis. The kidneys, testicles, less often lungs, digestive tract, liver, bones and joints are more often affected from visceral organs. The general condition is disturbed, cachexia and septicemia are increasing.
The diagnosis is confirmed bacterioscopically and culturally.
Treatment: iodine preparations, amphotericin B, orungal, nizoral, fluconazole.
Chromomycosis is a deep mycosis caused by fungi of the genus Hormodendron with a relatively benign course. It is characterized by the lesion mainly of the lower extremities, where at the place of introduction of the pathogen appears saturated red hump color, which grows slowly, accompanied by the appearance of new elements (hump shape) that do not merge with each other. In case of their fusion, deep infiltration is formed on the skin in the form of a conglomerate of tubercles, which rise sharply above the skin, are removed with the formation of extensive papillomatous sprawl, alternating with sites of necrosis, separating the blood-blue fluid (papillary ulcer form). Less often observed the formation of nodes (gummosis form).
The diagnosis is confirmed bacterioscopically and culturally.
Treatment: cryotherapy, surgical dissection, electrocoagulation, intravenous iodine preparations, amphotericin B in the form of tingling, orungal.
Prevention of deep mycosis is to prevent and timely sanitation of micro-injuries.
Pseudomycoses
Pseudomycoses include erythrazm and actinomycosis, which previously belonged to fungal processes, but a more detailed study of the pathogens allowed to classify them as special microorganisms that occupy an intermediate position between fungi and bacteria.
Erythrazma
Erythrazma is a very common disease of skin folds.
Etiology and pathogenesis. The causative agent of Erythrazma is Corynebacterium minutissum, it is detected in epidermis scales in the form of thin weakened septum threads, between which coccusoidal cells are located. The development of the disease is facilitated by increased sweating, failure to observe personal hygiene rules, as well as high temperatures and humidity in the environment. It is mainly men who are sick. Contagiousness is small.
Clinical picture. The most frequently affected are inguinal and hip folds, armpit pits, contact surfaces under the mammary glands in women. At the same time, centers of erythyroidism may be on the torso, limbs (including interfinger folds and vaults of feet) and even on the foreskin and head of the penis. In men, the usual and very typical localization is the areas of the inner thighs adjacent to the scrotum (scrotum is almost never affected). In these areas, sharply delineated spots of non-inflammatory character appear, whose color varies from yellowish red to red-brown. The spots are rounded, ranging in size from dotted to the size of coins of different value; when the spots merge, large centers with festoon contours are formed - up to the palm and more. The surface of the initial rashes is smooth; with time a slight flaking with small scales joins.
Subjective sensations are absent. Under the influence of high humidity, friction and secondary infection joining, the centers of erythritis in the folds, especially in summer, are complicated by inflammatory phenomena (hyperemia, swelling, rejection of the stratum corneum) up to the formation of oprela, accompanied by itching.
The diagnosis of uncomplicated erythritisms does not cause difficulties and is based on the clinical picture. It is confirmed by the coral-red glow of lesions (due to water-soluble porphyrin. produced by bacteria) in the rays of the Vood lamp. Microscopic examination of scales is performed if necessary.
Treatment: 5% erythromycin ointment (light rubbing in the hearths 2 times a day for 7 days), 5% salicylic and 5% glycerine-salicyl alcohol, with common forms - erythromycin inside 0.2 ) 5 times a day for 5-7 days. Aqueous solutions of aniline dyes are used to eliminate the adjoining opalescence. The prevention consists in the hygienic content of the body, thorough drying of the skin, especially folds, after water procedures; removal of hyperhidrosis.
Actinomycosis
Actinomycosis is a chronic infectious noncontagious disease affecting humans and animals caused by actinomycetes.
The disease is observed in all countries of the world. Patients with actinomycosis account for up to 10% among patients with chronic tone processes. Men are twice as sick as women, the age of patients ranges from 20 to 40 years.
Etiology and pathogenesis. The causative agent of actinomycosis - anaerobic radiant fungi - actinomyces israeli, more often. The hypothesis of endogenous infection, in which the radiant fungi that constantly saprophyte in the body (in the oral cavity, gastrointestinal tract, upper respiratory tract), acquire pathogenic properties, is most recognized. The emergence of the disease contributes to the weakening of immunity, chronic infections, hypothermia, etc. Protective properties of the mucous membrane are violated due to local inflammatory processes, micro-injuries. Exogenous infection of open injuries, the development of actinomycosis in the epithelial coccyx, bronchial fistulas with subsequent spread to the surrounding tissues is also possible.
Around the introduced pathogens in the submucosal layer or subcutaneous tissue is formed a specific granuloma - actinomycoma with decay and suppuration and the formation of scar tissue (cartilaginous).
Clinical picture. Actinomycosis affects the respiratory organs, digestive tract, pararectal tissues, genitourinary organs, bones, skin. Actinomycosis of the skin may be primary and secondary and takes the form of several forms (nodular, bumpy, ulcerative, etc.).
Nodular form of actinomycosis is characterized by the formation of a dense, low-movement painless node with a diameter of 3-4 cm or more, which, as it grows, protrudes above the level of the skin and is soldered with it, which makes the skin dark red with a violet shade. New hearths may form nearby. Nodes are prone to absconding and the formation of fistulas, through which the purulent content is poured out, often with yellowish grains - druzes actinomycete. Some fistulas are scarred, others appear again. The process has a persistent chronic perennial nature and is localized mainly in the cheek, chin, lower jaw, perineum, buttocks. In the lumpy form, which usually develops in the primary actinomycosis of the skin, rashes are dense, hemispherical dark red lumps with a diameter of 0.5 cm, which do not merge with each other and open with the release of a drop of pus from the resulting fistulous passage and covered with brown-yellow crusts. The process tends to affect subcutaneous tissue and spread to neighboring topographic areas.
An ulcer form is noted in weakened patients who have ulcers with soft subdued jagged edges and sluggish granulation at the bottom in place of abscodized infiltrates.
The diagnosis is based on a clinical picture confirmed by a bacterioscopy and culture.
Treatment: actinolysate intramuscularly in 3-4 ml or intradermally from 0.5 ml to 2 ml 2 times a week, for a course of 20-25 injections, immunocorrectors, broad-spectrum antibiotics (in case of secondary infection). surgical dissection of lesions with subcutaneous tissue.
By: Dr. Cindy Li